Mad dogs and Welsh children
It must have been terrifying. One moment the children were happily immersed in a game; the next, they looked up to see a furious hound bearing down on them, snarling and slathering.
In my beloved Welsh granny’s trove of stories, few sounded quite so frightening as the rampage of the mad dog. I had heard the century-old tale many times over the years, but it was only during the Covid-19 pandemic, locked down in Paris with disease on my mind, that I dug into the history myself.
It began in the summer of 1899, when my grandmother’s uncle, the wonderfully named Vavasor – aged six at the time – was playing with friends in their village of Pontarddulais in South Wales. The little settlement on the fringes of the coal-rich Welsh Valleys was in the throes of transformation, with a series of tinplate mills springing up and the population swelling with migrant workers.
On this stifling day in late July, an “infuriated” dog came tearing through the streets and launched a frenzied attack on the group of children. Vavasor and his friends suffered “terrible injuries” according to the first, somewhat sensational account that appeared in newspapers around Britain:
 Manchester Evening News, 27 July 1899 (Newspaper image © The British Library Board. All rights reserved
Manchester Evening News, 27 July 1899 (Newspaper image © The British Library Board. All rights reservedLater reports mentioned no lost eyes but the injuries were nevertheless alarming: seven boys and a girl, aged two to ten, had been bitten – Vavasor on the arm, and two of the younger boys on the face.
The children’s families were terrified, suspecting rabies. By the late 19th century, people knew only too well the potentially lethal consequences of a dog bite and the agonising fate of those who contracted the disease, then known in humans as hydrophobia.
The virus spreads by way of the nervous system to cause infection of the brain, almost always resulting in death once the horrifying symptoms emerge, from hallucinations to convulsions. The body of the Pontarddulais "mad dog" was sent to London for tests and local dog-muzzling orders were enforced, according to the press. But what could be done for the children?
 A mad dog on the run in a London street: citizens attack it as it approaches a woman who has fallen over. Coloured etching by T.L. Busby, 1826. (Wellcome Collection, Public Domain Mark)
A mad dog on the run in a London street: citizens attack it as it approaches a woman who has fallen over. Coloured etching by T.L. Busby, 1826. (Wellcome Collection, Public Domain Mark)
Fourteen years earlier, in Paris, Louis Pasteur had successfully but discreetly tested his rabies vaccine on a human for the first time, when nine-year-old Joseph Meister from Alsace was brought to him severely bitten by a crazed dog. There appeared to be little to lose. Over ten days, the boy was injected 13 times with increasingly virulent spinal cord matter from rabid rabbits. He survived.
As rabies has a relatively long incubation period, the idea behind the post-exposure treatment was to build up immunity before the disease took hold.
After success two months later with another badly-bitten patient, a 15-year-old shepherd, Pasteur went public with his vaccine to global excitement – and some criticism. Three years later he opened the Pasteur Institute, expanding his research on infectious diseases and offering free rabies inoculations to patients from around the world.
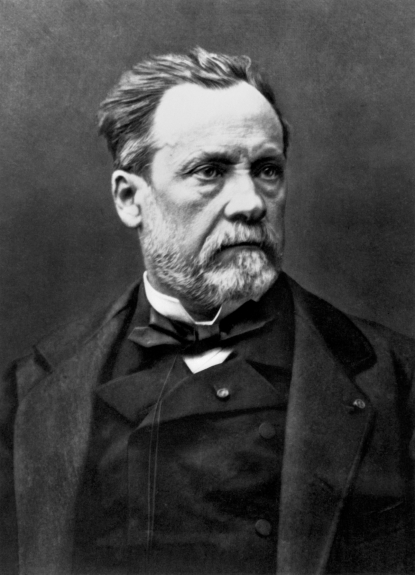 Undated portrait of Louis Pasteur (1822-1895), French chemist and microbiologist. (AFP)
Undated portrait of Louis Pasteur (1822-1895), French chemist and microbiologist. (AFP)
His breakthrough with the virus “was a game-changer – there was huge visibility associated with it,” the current president of the Pasteur Institute, Professor Stewart Cole, told me from his office on Paris’s Left Bank. As it happens, Cole is also Welsh.
“Because [rabies] was a huge public health concern in those days, the French public were immensely grateful and probably also proud that a Frenchman had come up with a wonderful ‘cure’. And so this led to a sort of early crowdfunding initiative that appealed to the public generosity,” he said of the institute’s financing. Even foreign dignitaries including Emperor Pedro II of Brazil chipped in.
 A detail of a mosaic on the ceiling of Pasteur’s crypt at the institute in his name in Paris (AFP / Stephane De Sakutin)
A detail of a mosaic on the ceiling of Pasteur’s crypt at the institute in his name in Paris (AFP / Stephane De Sakutin)
By 1899, Pasteur had died a scientific hero, and news of his institute and its life-saving treatments were closely followed across the English Channel. But was it safe, or even necessary, to send over the young Welsh children?
First was the question of whether the dog was really rabid. More than a week after its rampage, press reports said tests on the animal’s body were still inconclusive.
Though fear of the disease gripped the era, the actual number of human rabies deaths was not large in Victorian Britain, and London’s Star newspaper argued that Pasteur’s treatment posed a “serious risk” to the children. “There is no proof that the... dog was mad, for it is well known that the examination of the brain is not a satisfactory test,” said the editorial, quoted in other newspapers.
 A cartoon in the Western Mail ridicules the killing of the ‘mad dog’ and subsequent dog-muzzling rules (Newspaper image © The British Library Board. All rights reserved.
A cartoon in the Western Mail ridicules the killing of the ‘mad dog’ and subsequent dog-muzzling rules (Newspaper image © The British Library Board. All rights reserved.
Other critics argued that the dog should have been kept alive to prove it had rabies, although one wonders if they had ever tried to wrestle with a child-savaging animal.
Agricultural officials recommended the wounded Vavasor and his friends be sent to Paris as a precautionary measure. A local Welsh board of ‘guardians’ – tasked with supporting the poor before the birth of the welfare state – agreed to pay the expenses.
It was a daunting expedition for the little medical tourists: nearly 24 hours of travel by rail and sea, then invasive daily treatment that would last a fortnight – or three weeks for the boys bitten in the face.
 Picture dated November 1938 of the Pasteur Institute, in Paris. (AFP)
Picture dated November 1938 of the Pasteur Institute, in Paris. (AFP)
Why, by 1899, did Britain not have its own treatment facility? The main reason was nationalism, science historian Professor Michael Worboys told me.
“The British didn't want a Pasteur Institute proving that French science was better than British science,” said Worboys, co-author of Mad Dogs and Englishmen: Rabies in Britain, 1830-2000.
The second reason, he said, was Britain’s active movement against experiments on live animals, which were central to Pasteur’s laboratory work.
 An 1885 wood engraving depicts Louis Pasteur (left) watching a colleague trephining a chloroformed rabbit during his research on rabies vaccines (Wellcome Collection, Public Domain Mark)
An 1885 wood engraving depicts Louis Pasteur (left) watching a colleague trephining a chloroformed rabbit during his research on rabies vaccines (Wellcome Collection, Public Domain Mark)
British anti-vivisection campaigners championed alternative rabies “treatments”, such as one known as the Buisson system – recommended for the Welsh children by the London Star. “Essentially you put somebody in a Turkish bath and steamed the ‘poison’ out of them. Sometimes people died in the extreme heat,” Worboys said.
Perhaps unsurprisingly, medical pilgrimages to Paris had become common for dog-bitten Britons by the end of the 19th century.
 Pasteur commemorated in a lithograph by H. Meyer, October 1895 (Wellcome Collection, Public Domain Mark)
Pasteur commemorated in a lithograph by H. Meyer, October 1895 (Wellcome Collection, Public Domain Mark)
And so the Welsh youngsters set off by train from the nearby town of Llanelli, seen on their way by a host of friends and family assembled on the platform. Chaperoning the children was Vavasor’s father, David Lloyd Morgan (my great-great-grandfather), a Congregational minister.
“We left... in the best of spirits, although where and what sort of place we were going to was to me a perfect blank," he told Welsh newspaper the Western Mail. "None of us knew anything of France or the language, and the people and their habits were equally strange to us."
 The eight children who were bitten by the ‘mad dog’ and vaccinated in Paris (Newspaper image © The British Library Board. All rights reserved
The eight children who were bitten by the ‘mad dog’ and vaccinated in Paris (Newspaper image © The British Library Board. All rights reserved
But Lloyd Morgan’s trepidation over the voyage had nothing on his fear that his son might have rabies.
“I was terrified beyond conception. I possibly took the matter too seriously, but knowing that my own flesh and blood was in danger of that most awful disease, and fully realising the painful and heartrending stages through which it pursues its deadly course, my condition was a sad one,” he said.
“I slept with him each night after he had been bitten, and before leaving for Paris I frequently used to wake at all hours of the night and jump out of bed, fancying I could hear dog-barks and all manner of noises. Those were the most terrible nights I ever experienced.”
 The Rev. David Lloyd Morgan, who chaperoned the bitten children, including his son Vavasor, to Paris. He said he suffered his ‘most terrible nights’ before the trip (Photo courtesy of Susan O’Brien)
The Rev. David Lloyd Morgan, who chaperoned the bitten children, including his son Vavasor, to Paris. He said he suffered his ‘most terrible nights’ before the trip (Photo courtesy of Susan O’Brien)
On arrival at the institute, Lloyd Morgan was impressed. “The native Frenchman has no privileges beyond those extended to foreigners, and the physicians are courteous and obliging to all who enter.”
Along with the children in the queue were soldiers and an army officer all the way from India, one of them bitten by a jackal. Even these battle-hardened men were said to emerge from the treatment with a “drawn look” on their faces.
“It wasn’t like getting your Covid jab when you're given a tiny amount of vaccine. They’d be giving them five or ten millilitres,” Worboys said. “It was more like a modern surgical procedure.”
 Old medical devices displayed at the Pasteur Museum in Paris (AFP / Stephane De Sakutin)
Old medical devices displayed at the Pasteur Museum in Paris (AFP / Stephane De Sakutin)
The French physician struggled to comfort the Welsh-speaking children as their knickerbockers were unbuttoned for the operating room. “The patient was then taken on the doctor's knee, with his legs firmly gripped by the doctor's knees, while the arms are pinioned in the vice-like grasp of an assistant,” said Lloyd Morgan.
“The physician afterwards takes hold of a fold of the abdominal flesh, and receiving the injecting syringe (resembling a needle) from the assistant, forces into the flesh.”
 A doctor vaccinates a patient against rabies, at the Pasteur Institute, 06 November 1938 in Paris. (AFP )
A doctor vaccinates a patient against rabies, at the Pasteur Institute, 06 November 1938 in Paris. (AFP )
Reluctant eight-year-old Stanley Howells was first in line. “The other children, hearing their comrade shriek, came to the conclusion that, like the rabbits, he was being killed”.
Understandably, the doctor “came in for a great deal of abuse” from his small patients, who nevertheless returned daily for the same ordeal, bribed with promises of fruit and coins, their chaperone said. “If it had not been for a plentiful supply of plums I don't know what we should have done.”
 The Pasteur Institute’s record of Vavasor Morgan’s treatment in August 1899 (Musée Pasteur)
The Pasteur Institute’s record of Vavasor Morgan’s treatment in August 1899 (Musée Pasteur)
I was delighted to find these detailed chronicles in the online British Newspaper Archive, including the rare photograph of the eight children together – the first I had seen of Vavasor, who peers into the camera from a huge Victorian collar.
Archivists at the Pasteur Museum also dug out the medical logs from the group’s trip to Paris, in which the doctor’s scrawl notes their injuries, daily treatment and the fate of the dog.
The non-profit institute has continued to further Pasteur’s legacy over the decades: developing various new vaccines, producing typhoid jabs for First World War troops, and, in 1983, discovering the HIV virus that causes AIDS.
 A laboratory technician works on the genome sequencing of the SARS-CoV-2 virus and its variants at the National Reference Centre (CNR) for respiratory viruses at the Pasteur Institute in Paris on January 21, 2021 (AFP / Christophe Archambault)
A laboratory technician works on the genome sequencing of the SARS-CoV-2 virus and its variants at the National Reference Centre (CNR) for respiratory viruses at the Pasteur Institute in Paris on January 21, 2021 (AFP / Christophe Archambault)
Early last year, it became the first European institution to sequence the whole genome of the new coronavirus, a crucial step for scientists to begin developing testing and potential treatment.
But in January, to much disappointment in France, the institute abandoned its main Covid-19 vaccine project after failed clinical trials.
Cole said that, while they were ‘“very strong” in areas like epidemiology, “we realised we didn't have enough critical mass working in the area of vaccine development”.
“We need to be… trying to be foresighted and see what's around the corner, what could be the next source of a major epidemic or pandemic.”
Wales, a nation of three million people, has been a world leader in the speed of its Covid-19 vaccine rollout. By July 22, around 70 percent of Britain’s adult population, and more than half of the European Union’s, had been fully inoculated against the virus.
But the same could be said for just 1.5 percent of people across Africa, according to the UN. “We should be more effective than we are now,” said Cole. “It is a bit shocking, the disparity.”
 A healthcare professional administers an injection of Moderna Covid-19 vaccine at a vaccination centre at Ffwrnes Theatre in Llanelli, South Wales, on April 9, 2021. (AFP / Geoff Caddick)
A healthcare professional administers an injection of Moderna Covid-19 vaccine at a vaccination centre at Ffwrnes Theatre in Llanelli, South Wales, on April 9, 2021. (AFP / Geoff Caddick)When Vavasor needed treatment, the fact that the Pasteur Institute administered vaccines to anyone in need was lauded hundreds of miles away.
"That the latest Continental development of science should be accessible to the poor of a Welsh village is of itself a comment upon the rapidly progressive age in which we live," said a Western Mail editorial.
The “brave little Celts” eventually returned home in stages, looking “far more cheerful and happy than when they left” – to much rejoicing among their families and local celebrity status.
“If a few tears were shed and a slight tendency to flinch showed itself at the last moment, they certainly had displayed a pluck and stoicism which might have reflected credit on many an older person,” said the South Wales Daily News.
More than a century later, and with fear of a very different virus gripping her rural community in North Wales, my 70-year-old mother – Lloyd Morgan’s great-granddaughter – was able to drive ten minutes down the road for a safe and quick Covid-19 vaccination in the arm. She didn’t even need a plum.
 Rachel O’Brien after her first Covid-19 jab, just outside central Paris
Rachel O’Brien after her first Covid-19 jab, just outside central Paris
Here in Paris, I thought of my ancestors’ adventures as I jumped on the metro and rode a few miles across the city to get my jab – in a hall around the corner from one of thousands of French streets named after Louis Pasteur.
“But you went such a long way!” said a neighbour when I returned to my own quartier that afternoon. I disagreed.
With thanks to The British Newspaper Archive. (www.britishnewspaperarchive.co.uk).


